The following post is about how myself, my partner and the police called upon the Leicestershire Partnership NHS Trust (including the Community Mental Health Team) to help my partner when she when she was a danger to herself.
My notes here start around one and a half weeks after she had been discharged from hospital (whilst mainly being under Section 3 MHA, her stay was roughly 8 months in total, disrupted recovery with a rushed discharge). No special provision had been made to support her at home apart from a bi-weekly meeting with her Community Psychiatrict Nurse who has still yet to get to know her properly and had ignored her previous plans of a suicide attempt. Also there was the possibility of referral to an Occupational Therapist (who apparently are very rare in CMHTs in Leics).
J’s care plan states that if she is in crisis within working hours, she is to contact her CPN at the CMHT, or see her GP, and if out of working day hours, contact an out-of-hours GP service. Failing that she would have to go to an NHS Walk-In Centre, or present herself at the A&E dept in a nearby Leicester, where she could patiently wait to be seen by the City Crisis Team.
Her situation may have been complicated by the fact that she has had some particularly bad experiences in the past to the County Crisis Team (now called the Home Care Treatment Team or something, because they clearly had to drop the word “crisis”). I’d like to add that in my experience working in the mental health drop-in centres the reputation of the Crisis Team and their phone service is particularly bad amongst the service-users - almost as they were the least sympathetic, least empathetic, zero “people skills”, barely qualified pig-ignorant robots to work in mental health care, and I am being polite. Of course there were exceptions, the occasional good, never to be heard from again, part-timer… Anyhow, they have mixed reviews, so you can’t blame J for thinking she’d rather be dead than actually talk to the County Crisis Team. This is a moot point, because the Crisis Team will not talk to you unless you have been seen or referred by a professional like a doctor or CPN within the last 24 hours. Basically, you can’t talk to them even if you want to when you need to. Also, they are the gatekeepers to MH hospital. They even frustrate the consultants. Imagine the worst person in your family for opening up to, crossed with the harsh brusqueness of a surgery receptionist. That’s my personal experience of the County Crisis Team, and it matches pretty well with the anecdotes from mental health service-users I have met at work. I’ve digressed.
My partner, J, was one and half weeks out of hospital. She was trying to sort her possessions so that she could resettle and start her new post-ward life. This sorting was becoming frustrating for her, seemingly unending and impossible. The suicidal thoughts have never really left her, but their intensity had increased again. She had an appointment with her CPN the following week and we tried all sorts of distractions to get her through until then. I think at the weekend she tried calling Samaritans and the local Focus Line. It was all a bit hit and miss. I think sometimes they assume that because I am nearby that she will be magically safe. We don’t live together but just in case start to stay over again on a type of suicide watch.
I was still taking holiday after leaving my job in the drop-in, and so I had some time in the day and night to be with her. Often she doesn’t mention me to professionals for fear that they will not provide help.
We knew that she has an appointment with her CPN on Thursday and we just try to muddle through. I hoped that he would put a spin on things, signpost to a service or make a suggestion which will help her, or somehow divert the suicidal focus.
She had started to cut again. It’s a private act, she never discusses it unless I ask directly, and it’s a pretty short conversation. Self harm helps her cope, maybe it even keeps her alive. She starts obsessing about going to the local motorway bridge to throw herself off onto the fast moving traffic below - a method a friend was successful with. I secretly wish for the days when she was able to drink as well, but she has been tee-total for well over a year now.
I remember it being a struggle walking through the busy market day to the CMHT for the CPN appointment. She tells me afterwards that she had explained to the CPN how badly she was feeling. I don’t remember if she said that he had offered extra help. CPNs can be strange, one minute they can make things happens by way of referral or phone calls, and the next they say odd things like “my hands are tied” or “what would you like me to do?”
She was still pretty unwell after the appointment and we try to get through hour by hour back at her place. By 4pm she’s absolutely determined to end her life and I ask her to try everything that is written in her care-plan. 4pm is a deadly time depending upon which services are open or closed. She rings the CMHT. The on-duty CPN rings back and tells her that she needs to talk to her GP or an out-of-hours GP, or maybe go to an Urgent Care Centre (I’m not sure about the last bit being actually said, but there’s a logic to this that rings true with previous care plans).
J rings her GP surgery. There is some confusion on the part of the receptionist. J is offered an appointment on a different day or maybe a call-back from a nurse. I think the nurse called back and was also confused (I can’t remember the details). J is not happy and scared by the choice of doctor for the appointment (he had previously tried to section her on the spot). The trouble here may have been that had we waited another hour or so, an emergency doctor call-out may have been possible through the Out of Hours GP Service. Somehow, it becomes clear that our next option is to go to the NHS Walk-In Centre, now relocated away from the town centre and renamed “The Urgent Care Centre”.
We call for a taxi and travel to the Urgent Care Centre (run by a Nottingham Trust). J fills in a form which appears to cater for only the simplest of ailments - it’s a type of computerised triage procedure. Some time passes on plastic chairs. J wants to leave immediately to kill herself. I think I convinced her to sit and wait. We are called in to see a nurse. After much to-ing and fro-ing with a colleague, we are told that we can’t be assessed in the Urgent Care Centre and have to go the A&E dept at the LRI in Leicester. A while back it was policy for professionals to come out to the walk-in centres as they were considered to be safe places to wait, this would include the County Crisis Team. There isn’t even a doctor at the Urgent Care Centre. We remember the 8 hour wait we had in A&E once only to have a patient queue jump in front of us in EDU because the City Crisis Team recognised them and not us. The City Crisis Team are different from the County Team, but sometimes this just means there are less knowledgeable as to who your local services are.
J starts to panic, she’s had enough, she is determined to end her life as soon as possible, she’s only been doing this to appease me. She often tells me that she never wants to hurt me, but that she can’t just stand to live any longer, that it is too painful, so why can’t I let her go?
The staff at the urgent care centre talk about providing us with transport or even calling an ambulance. By this time J is already leaving, I follow. Powerless, a nurse calls after us, “If you leave now, we will have to call the police” J is pushing onwards back through the doors to the waiting area. I think I remember looking around at the nurse, half shrugging, I can’t remember, maybe I just mentally agreed with the nurse, slightly pissed off that this was the best solution to our problems. Their call. J was seriously triggered, she was my problem for now.
We have a long frantic walk up alongside a dual carriage-way. J is wanting to catch a bus to motorway but also looking at the traffic, as if willing it to be busier so she can throw herself under a vehicle. I know that J’s low energy and anxiety-knotted back will give out at some point. I’m partly there to catch her when she falls, partly there to physically block her like a basket ball player when she wants to run into danger. I’m tempted to tackle her and just sit on her, but this might cause more distress and injury. It’s frightening how logically all this seems in such an absurd and frightening situation.
The police catch up to us in a car. They sit us in the back of the car, she tries to escape by winding the window down and opening the door from the outside (she tries this later too). J keeps saying she doesn’t want to go to A&E and doesn’t trust the Crisis Team. Police take us back to Loughborough’s new police station but we have to stay in car. They bring us water.
Eventually the Liaison & Diversion Service arrive in their “special van”. This is a new pilot scheme where police and mental health work together. Much celebration has been had in the local media over Leics being one of a handful of chosen counties for the pilot project. They are a welcome alternative to going straight to A&E in Leicester, or an assessment by the County Crisis Team on site, but we’re not really calling the shots here. I just hope J will be kept safe from harm.
We are allowed into the new police station, to go into an interview room. Apparently the loos are out of commission, as is the boiler which provides the police with tea and coffee. It’s fairly late. In the room is the specialist police officer and the specialist mental health worker (on secondment from LPT NHS) The mental health worker is V. She is pleasant and chummy. For some of the meeting she seems to “get” J. J tells them that she feels guilty for wasting other people’s time and finds it difficult to ask for help. At one point we even joke and swap photos of pet cats on our phones. J is told to “hang on” for 24 hours whilst V promises she will phone or fax CMHT, perhaps asking for more support. The L&D team seem understanding and sympathetic to J’s anxieties about services, but still, despite all this, she wants to kill herself (and isn’t safe to be left alone). Two other police give us a lift back to J’s place. It’s pretty late, I can’t remember the time. At least we got to make sure that the cat still well fed and sorted out her litter tray. I think we ate something, she went to bed, I stay on the sofa.
On Friday morning, I think we were waiting for a phone call from the CMHT. I guess that J was trying to get from hour to hour. I thought that we were coasting and surviving, and still a bit confused about the encounters from the previous day. But J is still planning. I probably said lots of patronising things about distractions and worksheets that used to help J from previous therapy. Randomly, I received a phone call from a delivery man trying to drop off a parcel. I live just up the road. I leave Jo for what will hopefully only be half an hour at the maximum.
When I return she is dressed. J mainly wears pyjamas in the house, outdoor clothes mean appointments, shopping or cafe dates. She was hoping to have left before I had come back. She leaves the house and locks the door behind her in order to slow me down.
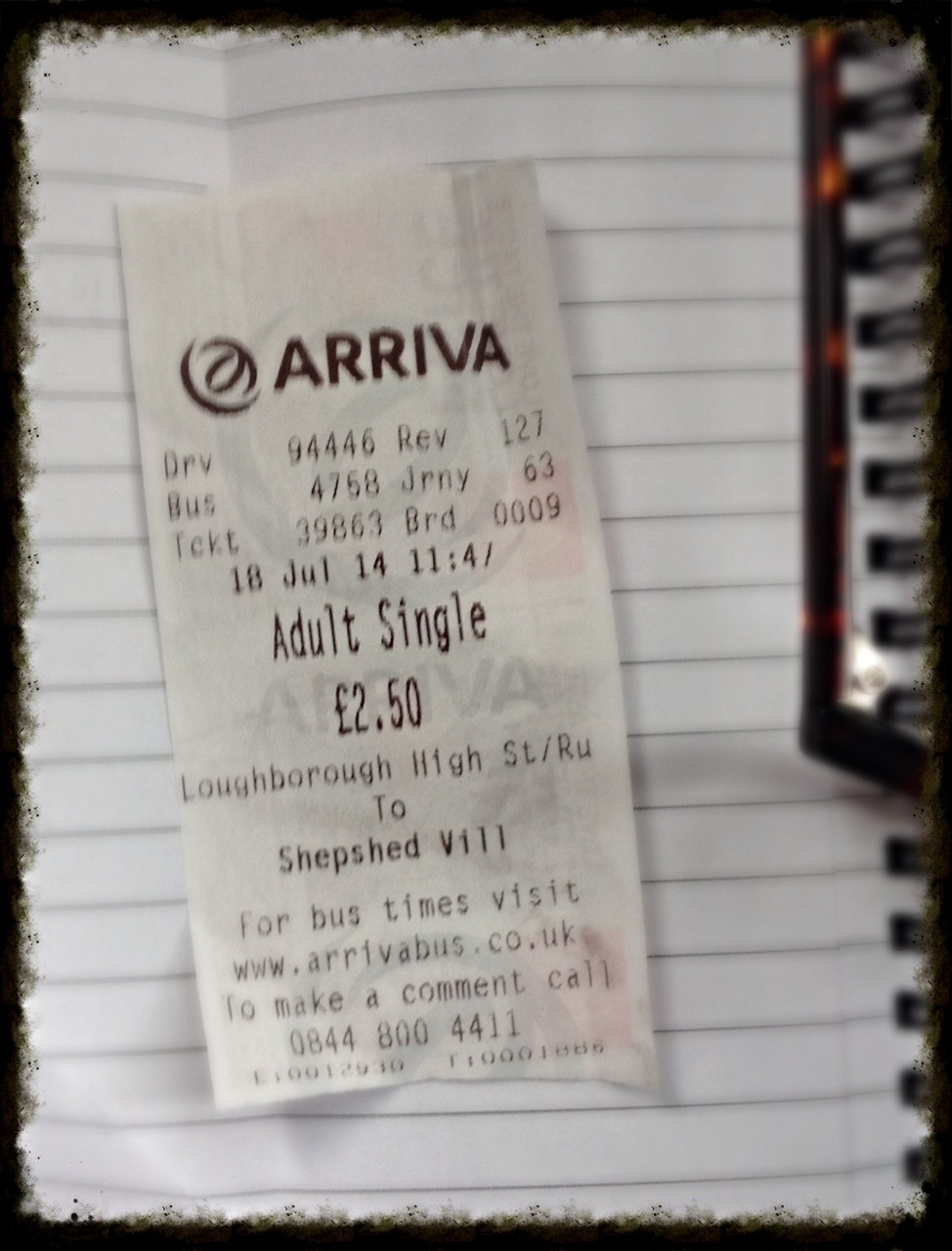
I follow her out and call police, who stay on the line whilst we wait and then she boards the number 127 bus. She asks specifically for the stop before the motorway bridge. I find myself buying a ticket to the same destination. Eight months previously we had been in an almost identical situation. Then I’d I pulled her off the bus, whilst trying to tell the driver that she’d planned to kill herself. After that we had chased about near busy traffic for another ten minutes in the street before help arrived. I think this time I felt that at least whilst she’s on the bus she’s in a contained space, also I was trying to stay calm and not provoke more distress. She sits down stays at a distance from me - I worry that it looks like I’m harassing her, which can freak other people out as well. She has a frightened wild stare. The police operator on the phone is all the time asking me where the bus is, what road it is on, the colour of bus and so on.
At a stop on the same dual carriageway where we were the night before I pass the phone to the driver, for the police to explain the situation. He then shuts the bus doors and explains to the passengers that there is a fault. We are to sit and wait for an engineer. Police arrive in a car, the doors open and Jo tries to run, is cornered, and corralled into the covered bus stand. They talk to her whilst she sits in the bus stand. It is hot, the sun bakes us through the plastic glass, we are both sweating. J usually sun burns easily - she is fair skinned and there is a medication side effect which means she can tan and burn quickly. She would never be out on a day like this. Her back is hurting her, I rub it to relieve the pain. She cries in desperation.
The bus drives off (I remember a strange dreamlike moment where I raise a hand, half wave a sort of “thank you” to the other passengers who look shocked and concerned, they wave back as the bus pulls away, as if saying “it’s okay, good luck, hope she’s alright” etc) The police are understanding but firm, I think Jo tries to run at some point and then we told to sit in one of the two police cars and are taken back to the new station.
We sit in a hot small foyer, the new carpet smells pungent like creosote. Police come and go, they swipe key cards (a bit like those used by nurses on the MH wards). Again, the new L&D Service arrive. This time they are different workers. I shall call the mental health worker “N”.
N knows J from 12 years previously from when N worked in the Crisis Team. Despite this, J tells me that she was actually one of the better workers. However, she patronizes J and tells her “not to be so negative”. She asks why she gave up singing or doesn’t go to church any more (she has done neither of these during our 6 year relationship, I feel that she doesn’t really know J at all, and wonder what they write in those files). She tells J that if she goes to the motorway bridge that she will be “arrested for wasting police time”. This upsets J and perhaps plants the seed for her change of suicide method later.
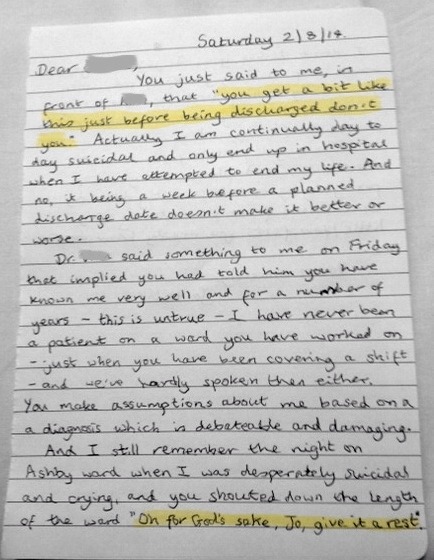
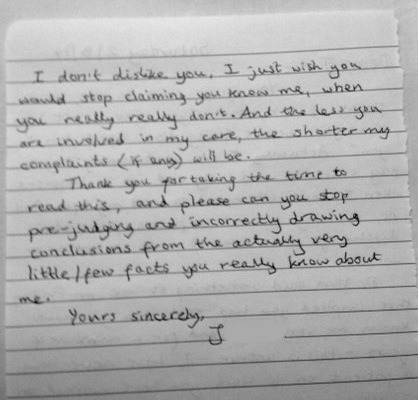
N says that J has a “robust” care plan to support her in the community, and that she has talked to the CMHT on the phone and says that J has an appointment with the occupational therapist to look forward to at the end of the following week. J does not know of this. No letter has been received and this seems irrelevant when the crisis is happening now (the Trust usually sends post second class, if at all). I partially agree with N that J might be experiencing a sort of “glitch” or spike where things seem much worse than normal and that there will be better times if J is able to wait, “ride it through” etc, but I do this only after it becomes clear that she won’t be readmitted to hospital. J is treated as though she is trying to manipulate the system in order to go back to hospital. It is two weeks since she first returned home. The previous long stay in hospital seems to be used against her - as though she is somehow she is dependent upon services.
We reiterate that J just wants to be dead and is a danger to herself. She hates hospital. N then tells her that she has to “make a choice”(?). Choose to live? This is confusing, but it is in line with how some professionals talk to patients they believe they have a certain type of personality disorder. It’s a despicable and disputed “Tough Love” technique. Somehow, J is supposed to take responsibility, or “own” her actions and be instantly in control of her feelings and emotions. This is like telling a person with a broken leg “to get up and go for a run”.
All this seems a little crazy, since J’s mind is not dealing in negotiable greys - it’s all black and white, and this relates to her OCD. She thinks in polemics (my word, not hers). For her it’s “Death” or “a life not worth living”. Fear and guilt might be factors in keeping her safe, not a love of life - she doesn’t want to hurt other people, especially those closest to her. None the less, the L&D team would rather gamble with the risk and suggest that she goes home, has “a cup of tea and something to nice to eat” and that will “make her feel better”. It’s clear that J’s 27-year history of anorexia and bulimia hasn’t registered in N’s reading of her file. This type of advice sounds not only like a dismissive platitude, but is alienating for J. It probably confirmed her suspicion of how little other people understand about her, or how little they care about fundamental details. J tells N repeatedly that if she can’t get to the motorway (for fear of arrest) that she will now go home and take an overdose, using her own medication, of which there is a lot.
J walks out of the foyer, frantic. I follow. A policeman shouts a name which isn’t mine, but he is addressing me. I was just furniture, I guess. They will catch up with us, apparently. We walk away from the station, Jo is nearly falling over. She sits on a rock in front of a gate. I try to console her and sympathize. J keeps saying that she’ll go home and take an overdose. At no point does this seem like a threat in order to gain access to hospital, but there is a touch of “fuck em all” defiance - i.e. she is has been wound up and provoked by the chat with N.
The van draws up beside us, we are asked to get into the area in the back. It’s floor seems very high off the ground. There are fixed benches and a table in there and nothing else. Exhausted, J struggles with little dignity to get up into the van. She falls back, I tear my jeans-shorts catching her. We get in, there are more nonsensical platitudes and small talk from N, and they take us back to J’s house. She keeps saying she’ll take an overdose. I think I’ve stopped listening to N, there’s something going on with road directions, I hold J. They drop us off in the street near J’s house.
We go indoors. For a moment I am feel relieved that we are away from the idiocy of that silly woman who clearly couldn’t give a toss about J. Maybe to N, J was some sort of template textbook cry-for-help cry-for-attention time waster, who’s risk of carrying through with her plans had barely registered. Or maybe once we were dropped off that we were no longer their problem and that they were now free to see their next case.
J immediately starts helping herself to her medication from a drawer. We fight over blister packs and she keeps putting handfuls of pills in her mouth. It gets fairly rough. I call the police whilst wrestling with her. By the time they arrive she has taken over hundred assorted pills of strong medication (worked out later from counting blister packs). Later a paramedic arrives - calls in an “amber call”. ECG are stickers applied to Jo, pulse is monitored and so on. J starts to get very sleepy. Before we eventually leave in an ambulance, there’s a strange moment when a police woman rather abrasively asks if J is going go in the ambulance without a struggle because there’s another important call they have to go to. J says she won’t be a problem, but I’m uncomfortable with the police revealing their priorities this way, especially when my partner might be about to die.
Then there follows the ambulance journey to hospital. J is disorientated, sleepy, fiddles with the trolley bed belt, she seems woozy, I think I remember an oxygen mask. When we arrive at A&E we are taken straight through into “Resus’”.
For many hours she is attached to drips and machines. She falls in and out of consciousness, a catheter allows fluid being flushed through her blood via cannulas to be urinated out. Apparently they don’t pump stomachs any more. She stays in the hospital for the night. A nurse later tells her that it was a “pretty close thing” or words to that effect. No-one explains much to me, but they ask questions, mainly about unspellable medication names.
I leave her bed at about 3am. Three taxi firms are not answering the phone. I walk through the Summer rain with ripped shorts and catch a taxi from in front of a nightclub in Leicester centre. I lie on the floor back at J’s place cuddling and apologising to the cat.
The following day when she was more conscious she tried to run away from the hospital, security find her and bring her back. Eventually a bed is found for her at the Bradgate Mental Health Unit after a country wide search (which I suspect never occurred). She is told she is lucky to have found a bed locally.
The admission to Bradgate is a whole story in itself, but we are still both left reeling at the number of missed opportunities there was to take J to safety - some of which were in the control LPT NHS employees.
One wonders what the police make of all this as well.