These were just a bundle of frustrations of experiences totally separate from requests or issues regarding my partner’s care. I had been planning for some time to provide general feedback on her previous admission with the hope that someone as the Leicestership Partnership Trust might want to make improvements (which sounds a bit pompous and naive reading that back). As a visitor-carer I felt pretty intimidated by things you’d expect to be quite the reverse in a therapeutic setting. As yet I’ve had no response to this - just an automatic email, but hey, it’s just general feedback.
___
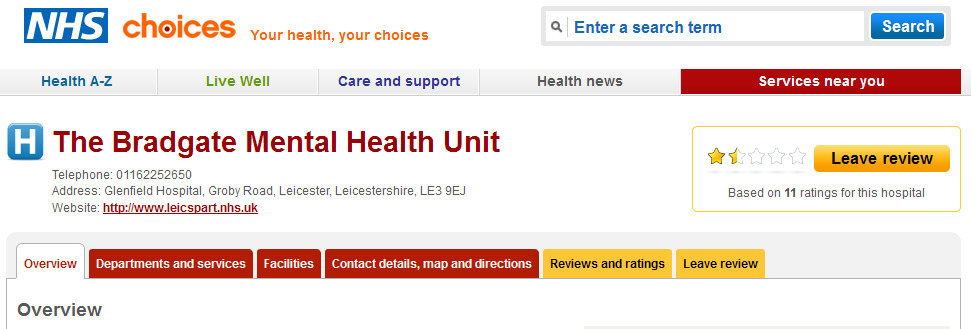
Hi
My partner recently became an patient again at the Bradgate Unit. This is email is a set of observations based mainly on my own experiences as a visitor (carer/next of kin) to several different wards. This is general feedback, just to highlight an awareness of issues and not a complaint. It is also not about her day to day care on the ward. Please feel free to forward to anyone to whom these issues are relevant (i.e. possibly hospital managers regarding building layout issues, amenities and the Head of Wards regarding staff the way staff address visitors in person or through corridor intercoms). The best way to reach me is through email if further views are sought.
W____ ______
(partner / next of kin for J_ _____, currently an inpatient on Bosworth Ward)
____ @ ___
_____________
A Lack of Visible Guidelines for Visitors
After eight months of my partner being on Ashby Ward (briefly staying on Beaumont Ward during building repairs disruption) , I pretty much felt that I understood visitor protocols at the Bradgate Unit. Upon her recent admission to Bosworth Ward, I am finding that every time I have visited that I have somehow broken a rule previously or am in danger of breaking a rule. I have been trained in the Protection of Vulnerable Adults (including awareness of carer and institutional abuse) and many different types of risk assessment in my previous work as a mental health drop-in worker. I am very sympathetic to the needs of the environment of a mental health ward with regards to keeping loved ones safe.
Apart from in the Welcome Pack (procured for my partner only after talking with a LAMP rep and not when she was admitted three days earlier) I see almost no rules or guidelines for patients or visitors on the walls as notices or in the form of leaflets. Examples would be: where are visitors allowed to go on the ward, under which circumstances should bags be searched, who to address when a named nurse is not available.
As with patients, when a rule is being broken it is very important that staff handle the situation in an unprovoking and respectful manner. Visitors are not telepathic and generally the do not wish to disrupt the harmony of the ward, nurses need to be reminded that what is normal to them in their work environment may in fact make no sense to an outsider. Also they may need reminding, as do patients and visitors, that different wards may manage situations differently - even if the end goal is the same, patient safety.
Intercoms and doors
There seems to be some confusion between different staff as to how to address people through the intercoms and then it’s hit and miss if they are able to activate the doors to make them open. The intercom buzzers also appear not to work at times - perhaps when another intercom is in use. This is especially frustrating if you are being kept waiting in one of those greenhouse-like corridors and the button isn’t even making a sound. Instead of operating the doors from the office, nurses will sometimes come out and use key cards (this would usually happen after a delay on both Ashby and Bosworth Ward). I very familiar with the silent green light which means the door was unlocked, so I don’t believe the problem is me pushing a door at the wrong moment, it seems more like a technical flaw or a misunderstanding on behalf of the operator.
Meet and Greet
Upon entering a ward there are small notices asking visitors to address “the receptionist”. This doesn’t make any sense. What receptionist? Where?
On Bosworth and Ashby Ward I’m not sure if this means I am to knock on the closed staff office door or address the nurses at the station/desk. (On Ashby Ward there was at least a sign inviting people to knock and wait) On the newly built Beamont Ward (where my partner was placed in the daytime during disruptive repair work to Ashby) I’m not sure if ever I remember seeing a person/receptionist in in the first bay - which was an issue when trying to leave the ward.
When addressed by staff at the door the ward, sometimes they will just stand there, silent, as if waiting for you to say something. A simple “Hello, how can I help you?” would help (this would also be useful over the intercoms, not just “Yes” or “Hello” or nothing at all). After I had been let on to the ward and walked towards the central area, where my partner was sitting, “Can I help?!” was used in what could only be described as a passive-aggressive threat. Maybe this is just people-skill thing. Nurses introducing themselves and saying their name may help too. I believe that the staff regularly forget what an strange environment the Bradgate Unit for any outsider can be. I have often been involved in my partner’s recovery (and care advocacy) and I have found that lack of the simplest courtesies can be alienating and will make even the calmest person defensive or even argumentative.
After several admissions of my partner to the Bradgate I’m finding that it’s still easy to confuse nurses doing “obs” with those who can help with a query - especially at a desk which might be the nurses station. Again clear directions for enquiry are required.
On a positive note, my partner and I still really appreciate that the nurses are in uniform. However, the signs regarding uniform colour and rank are baffling to me as to their relevance to non-staff (apart from the OTs and domestic staff who are clearly employed on the ward in a very different way). My partner is quick to say that many tasks can only be performed by staff of specific ranks (the distribution of PRN medication for example), but she has had to work this out for herself. None the less, it’s still good to be able to differentiate patients, visitors and clerical staff from the nurses quickly and a uniform helps with this, even if the badges are not on always visible. The photos in the hallway of staff is also a really marvelous idea for orientation.
Facilities for visitors
I really appreciate the new doors in the corridors and the cameras. My partner in the past had been able to run down the corridors and out of reception (at least twice previously). Now I feel she is safer and at times she’s told me it makes her feel safer from herself.
However, when visiting a patient who is confined to the ward, visitors must go through three locked doors and down three long corridors (from Bosworth) to be able to access one toilet (one for each sex) in Reception. Not since school have I had to announce my bladder intentions to so many people and be made to wait at doors. If there is to be any more more improvements to the building, may I suggest that visitor loos be made available in the atriums where the wards meet, i.e. not far from the wards, but still off-ward in line with infection control. I’m not sure what is like for elderly visitors, but I take medication which means that sometimes I need the loo more often than normal, and personally I think it’s a waste of staff time to be buzzing me through more than one door.
As always, drinks machines and refreshments for visitors could be improved with regards to availability and location. Perhaps a change machine could also be provided - as they are in Glenfield Hospital. For some reason the only bins in the reception foyer are in the toilets.
I am not including the Outpatients area or the Involvement Centre (I believe there’s a cafe) as part of visitor facilities as both areas are often closed in the late afternoon and evening (when visiting hours are). During protected mealtimes in the evening, relatives and visitors are corralled in reception, when they waiting to go in. Other places at least have a water cooler. Perhaps the Outpatients’ room with access to it’s snack and drinks machine could opened to the public between 6 and 6.30pm (protected mealtimes period). This may also distract confused and frustrated visitors who are trying to see loved ones but have been told to wait.
Again, a positive improvement last year was the provision of the sofas and plants in the reception area.
Thank you for reading.
W. ———— 24/07/14
—- @ ——