What do you mean when you say "carer"? Are you a family member or partner? Just trying to understand...
Query from lovemyesotericmind (Tumblr)
It took me a while to accept that I was a “carer”. It’s somewhat easier to state whilst my partner is a regular inpatient for mental health treatment. Foremost I am her partner, sometimes I am classed as “next of kin” - which can be a big deal when a person is Sectioned (forcibly kept in hospital) under the Mental Health Act, you become the officially notified person and you have a right to challenge the Section. In situations where her outpatient care is lacking, I have a real voice as her carer (and sometimes “advocate”), since it affects my life too. After that I am her partner (not quite common-law husband and wife because we live in separate small dwellings) After a few years of this (I have been J’s partner for seven years) and realising that I needed my employers to understand that occasionally that I must be available when J is in crisis, as well as compensating on a daily basis for J’s peculiarities resulting from her condition, I knew that I was her carer. In fact my current availability to employers is very restricted, because of my need to be available to her (also I can’t concentrate in any job whilst she is actively trying to kill herself). I’m trying to be self employed, but may have to make some difficult decisions soon (I despise contact with the brutal welfare system) In the UK there are some problems with the formality of the title, depending upon whether or not you can claim benefits depending upon the role. Politicians and charities are now acknowledging the “hidden army” of carers as a genuine saving on the NHS and Social Services, which can be vindicating in a way that it wasn’t in the past. Even when she isn’t in crisis, I prompt her to take medication and helping her to not worry about appointments, I do errands for her when she is agoraphobic, this includes picking up prescriptions and keeping her company during interviews, assessments etc. (Edit: I help with meals which can be an issue regarding her ED) I find the issue a confusing one, when you love a person, these are the things we do, it seems so normal. At some point, friends and colleagues starting talking about my needs, which didn’t make any sense to me, since I always felt that J’s problems were being barely addressed so it seemed bizarre that I could even identify myself as someone in a role defined by her illness. This is all very strange, because as a mental health worker in the voluntary sector (a job I’ve now left, partly because there was “mental health” in too many corners of my life and partly in protest at changes to local services), I was always signposting people to get support to alleviate whatever load life was throwing at them, and some of them were carers-in-denial too. Oops, sorry if I’ve babbled a bit. Talking about the role of carer is still something I’m negotiating with and am currently having teeny bit of a crisis with my job situation as well. ;) The good news is that I’m starting to get advice. Thanks for asking the question, it sometimes helps for me to see my thoughts and feelings written out like this. :)
Failing Mental Health Services in the UK is a blog written by an ex-mental health voluntary sector worker who is also a carer for a long term sufferer of mental illness. Links to news articles. Personal experiences and observations.
Sunday 26 April 2015
Wednesday 22 April 2015
A Better Day (J's care update)
By way of balance, yesterday was a better day. During my visit in the afternoon, J asked that her named nurse explain a traffic light warning method that had been suggested on the previous day. J is currently on Level 1 Obs (this is when a nurse has to be in line of sight at all times) - for J this is mainly to discourage her from the improvised ligaturing. The traffic light idea was basically a very simple way for J communicate her level of risk in an effective way without having to explain too much. What I liked about this is that we might be also able to identify the "light-amber" and even "green" moments, because when J is very depressed she can never recall when life was better, even if it was just the day before.
Slowly the our trust with staff is being rebuilt. As you know, if you've read the previous posts, when things don't go right I develop a hate-hate attitude towards consultants and specifically the whole of the Bradgate Unit who always have a lot of redeeming to do in my eyes.
J gets to see a new consultant tomorrow, hopefully a fresh start will do everyone good. J told me that the ward occupational therapist has agreed to work with her one-to-one since J sometimes struggles with joining group activities.
Again, I'm having to suppress the cynicism and over-protectiveness. We're still in limbo regarding J's possible extradition to the unit in Birmingham.
Yesterday morning I had some support for myself from a social worker from the local county council. On a practical and bureaucratic level there's not many options open to me as a carer whilst J is in hospital, but he did a fair amount of signposting to other organisations so that I get advice, and is prompting me to chat to a doctor about my own stress levels. I'm particularly freaked out at the moment that I may have dug myself into rut, financially and psychologically. Naturally this spills out when I'm trying to support J on the phone or in person, and frankly she really has enough on her plate to deal with.
Anyhow. It was a better day. I need to make sure I record the better days. Thanks for reading.
Slowly the our trust with staff is being rebuilt. As you know, if you've read the previous posts, when things don't go right I develop a hate-hate attitude towards consultants and specifically the whole of the Bradgate Unit who always have a lot of redeeming to do in my eyes.
J gets to see a new consultant tomorrow, hopefully a fresh start will do everyone good. J told me that the ward occupational therapist has agreed to work with her one-to-one since J sometimes struggles with joining group activities.
Again, I'm having to suppress the cynicism and over-protectiveness. We're still in limbo regarding J's possible extradition to the unit in Birmingham.
Yesterday morning I had some support for myself from a social worker from the local county council. On a practical and bureaucratic level there's not many options open to me as a carer whilst J is in hospital, but he did a fair amount of signposting to other organisations so that I get advice, and is prompting me to chat to a doctor about my own stress levels. I'm particularly freaked out at the moment that I may have dug myself into rut, financially and psychologically. Naturally this spills out when I'm trying to support J on the phone or in person, and frankly she really has enough on her plate to deal with.
Anyhow. It was a better day. I need to make sure I record the better days. Thanks for reading.
Friday 17 April 2015
Risks, MHA Sections and Consultant Sociopaths (update on J’s care at the Bradgate Unit)
So many things have been happening it’s hard to keep my head spinning at the same rate as events.
In the run up to her MHA Section 2 ending, the consultant must have decided that it was time for J stop wearing the seclusion gown (a special type of patient safety clothes) and to go back to wearing her pyjamas, like other patients on the ward. Nurses had a couple of discussions with her. Both times J said that she didn’t feel safe from herself. Triggering remarks included the mention that other patients shouldn’t have to see the impetigo on her legs and the burn bandage on her arm. J has serious negative body issues as it is. Then they insisted that they were returning the pyjamas to her anyhow, no matter what they said. They put the pyjamas on a shelf in her room and left. Shortly after J was found ligaturing with the pyjama bottoms around her neck. Later in a meeting with myself a nurse told me that the it had been “an acceptable risk” and that they “have to try these things”. I was pressing for decisions to be held back until J’s named nurse is present, and that when J shares her perception on risk that it is not a threat. Again, to J, this was an invalidating experience which somehow confirmed to her that she would be better off dead, especially since they were providing an opportunity.
In the meantime there were a few positive two-way chats with staff (including a service manager), but why do we need such near-miss situations in order to get to that stage of sharing. Patient centred care, my arse.
Suffice the say, the Section 2 ended and she was passed onto a Section 3 (up to 6 months). Again the doctors managed to do this in the clumsiest way ever. After five weeks of refusing to increase a low dose of a replacement anti-psychotic, the consultant finally admits to J that he doesn’t believe that she currently hears voices or hallucinates. They also said that she was going to be assessed and promptly sent to a specialised institution (Cambian again, Birmingham, PD specialists, 1-2 year stay). Naturally this was devastating and triggering. Fortunately this locum is in the process of leaving and good riddance to him. The other doctor was from a crisis team (surprise, surprise, the most prejudicial of all types of consultant). I pointed out of the phone to the AMP/social worker/CPN that, although I agreed to her being kept safe on the ward, that the Cambian residential stay was an old idea which both I and J have reservations about. Also with J challenging her diagnosis of BPD it may turn out to be a totally inappropriate referral. The AMP then managed to get the doctors to agree that the selection of services would be offered. In the meantime J constructed an argument that she was already being compliant with treatment on the ward and that there was still much to finish there. S3 has a “compulsory treatment” element. Both of us are unhappy that an original condition of her stay in hospital was for a complete drugs overhaul and that this had not occurred. This plan was even kept on hold by the locum, who didn’t believe that J needed medication at all. Much as I despise the Bradgate Unit for it’s lack of specialised therapists and dehumanizing battery-farming response to acute patients, H- Ward has been redeeming itself. All this is despite bullying from another patient and a list of day-to-day triggering problems (the pharmacy stopping drugs, attitudes of agaency staff, flaunting of basic privacy etc.).
J has been to Hell and back recently, sometimes begging to be let off the ward so she can end her own life (resulting in being called “selfish” twice by one nurse). I’m amazed she has any fight left in her, whilst still being suicidal.
Yesterday she was assessed by a worker from Cambian and she is now fixated with the not unreasonable notion that she’ll be whisked away suddenly and because of the Section 3.
I’ve come to the conclusion that all of the good professionals in her life spend 80 percent of their time repairing the damage caused by bad professionals. I’m also convinced that most psychiatric ward consultants are arrogant sociopaths. So much time and heartache is wasted on every ward stay because of her anxious responses to poor practice. I’m exhausted by trying the piece together the ongoing crime scene and calming her down, or arguing with her about things that might not be the best things to say to staff - for example, some stupid staff interpret explanation of SI and suicide plans as threats. Fortunately a majority of the shifts now have staff which have earn’t J’s trust. What really smarts for me is that when I was asked my opinion by a doctor a few weeks back, he was just assuming that I was being J’s puppet. Sometimes we need plain speaking as early as possible so we can get a second opinion and not waste time. That’s the good news, J is hoping to get a second opinion from a new doctors. There’s way too many “what ifs…?” at the moment.
Oh, and now the locum is leaving, the anti-psychotic drug has been put up to a useful level.
In my other life my concentration is now totally shot. Most of the time she is “safer” but not “safe”. Every other phone call might be news of her death as far as I am concerned. Lucy-cat is becoming my own positive prevention, i.e. to keep it together, stay well for both of them. I’m so tired of ignorant professionals. When nurses get to know her, they find her likeable and actually not all that complicated. So I have to blame the patient notes, a pile of meaningless Chinese whispers and generalisations passed between overpaid part-timers (the doctors).
Wednesday 8 April 2015
Alienation and invalidation still ongoing in her care (at Bradgate Unit)
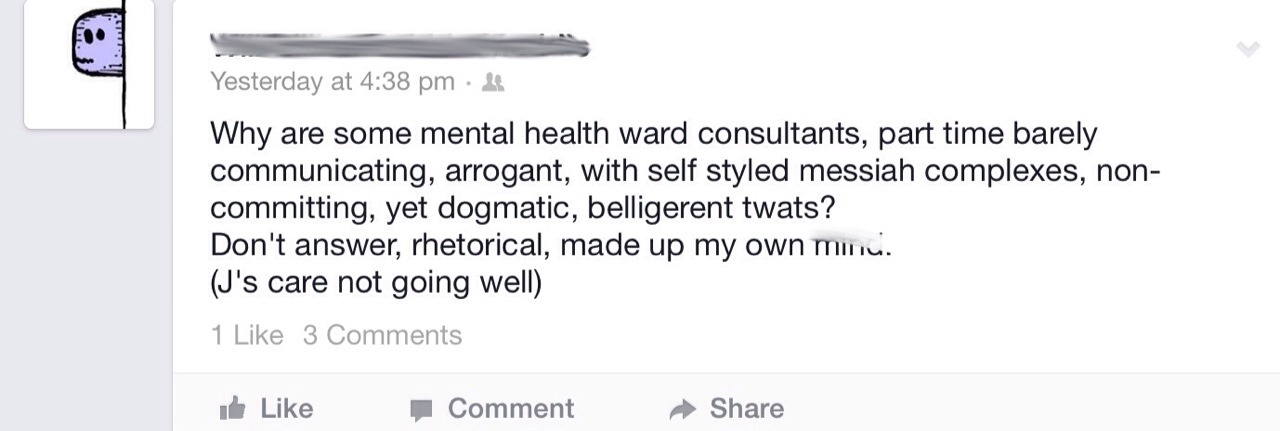
Sometimes I boil over on Facebook. This is a random status update of mine after J told me a whole load of stuff about her treatment today, including a nurse and a doctor inferring that J might not need to be on medication.
She is currently hearing voices screaming at her to kill herself and has hallucinations that she is surrounded by spiders, she is depressed, desperate to kill herself, and failing that, craves self harm.
One of the reasons why we agreed to her staying on the ward for six months was so that they can get her pills right. Does this sound like they’ve got the pills right and that she should come home?
Her MHA Section ends on 16th April. She says as soon as it is lifted that she plans to go the main road and kill herself.
I want her to have a second opinion, but we barely get to talk to the covering locum as it is.
Stupid man. Silly new ward matron treating J as though she “needs to take responsibility”
We’re going in circles, and she feels totally invalidated and more alienated. And this is before we even get on to all the other things which are happening, every one bad enough to be a trigger. Not to mention the bullying from another patient.
Hopeless. In every sense of that word. Stupid place. Stupid Bradgate Mental Health Unit and it’s record for helping patients to kill themselves by neglect and failure of duty of care.
Fuck them.
Thursday 2 April 2015
Update
I haven't posted for a while about J's care at the hospital. Many difficult things have been happening including her being sectioned for running for the door, a variety of types of self harm. There's a refusal by a doctor to increase her medication after taking her off other medication and there is ongoing bullying from another patient.
By way of contrast the nursing staff are being sensitive and compassionate.
I finally got to talk to a service manager about the road incident. But they feel we can't progress until she gets a statement from Dr D who is still away on leave.
J is now sectioned under the mental health act which means that contrary to what the care plan originally stated the staff are now willing to keep her safe when she is suicidal or in danger of self harm. This is a good thing. Because she has said that if she was given the choice to leave the ward she would immediately proceed to the nearby road in order to end her life. Despite saying this she is cooperating with her care but she does not believe recovery is possible. I don't want to write too much because I'm trying to save as much time for myself not worrying and thinking about mental health care all the time. It's very difficult for both of us at the moment. But hey we've been through so much already I guess that means we are both survivors.
Subscribe to:
Posts (Atom)