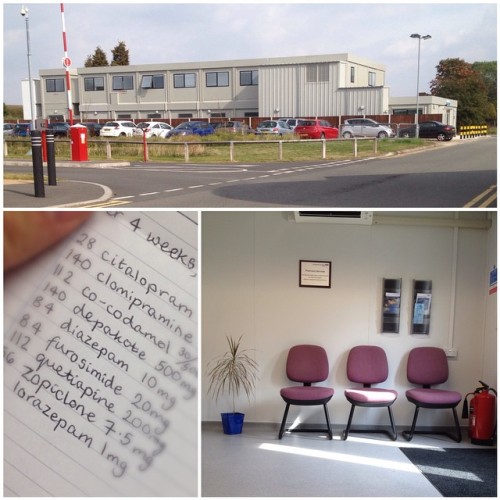
Article in Leicester Mercury on Saturday regarding the Bradgate Mental Health Unit and our experiences as carer and patient. 27th September 2014. (Yet to appear on the website, so please forgive the photos - click for larger views).
Incidentally to left is a photograph of me looking sad with the caption “ ‘It’s not making her better’ William Meddis, 42, who is concerned about the treatment his girlfriend is receiving at the Bradgate Unit.”
The More supplement in the Leicester Mercury is centred on “human interest” stories. J is very slightly fictionalized here, some generalizations have been rewritten as specific situations and so forth, but it communicates that sense of frustration we’ve had with the Leicestershire Partnership NHS Trust who run the Bradgate Unit. There’s some stats about deaths in there as well. I’m not sure I remember an agency nurse telling Jo to “pull herself together”, but it’s definitely the sort of thing I’d say about the attitude of some professionals we’ve met. It feels good that issues like incorrect medication upon admission were cited, because the head of the Trust has had to respond specifically to that, and she mentions the new pharmacy facility as an improvement (see earlier post where I had to go into the new pharmacy because of their failure to deliver to the ward and then getting stuck there whilst they corrected the prescription, incorrectly).
Interestingly, the Head of the Trust also says that they would be happy to meet with me. This is funny because letters sent to specific staff seemed to be responded to by Customer Service so far. Also, when someone says that they want to meet you in person it suggests that you went to the papers first, which is not the case.
You can read in this blog the two detailed letters of complaint I’d already sent to the Trust.
My complaint resolution deadline has been extended by Customer Services until mid October. So much for, “we will respond within 25 days”. Hopefully this is a good thing or maybe it just means that some staff are on holiday. ;)
My complaint resolution deadline has been extended by Customer Services until mid October. So much for, “we will respond within 25 days”. Hopefully this is a good thing or maybe it just means that some staff are on holiday. ;)
Edit: just reading the article again ... I have to say that when J is in crisis that I am a fan of "containment" or even sectioning because it can be the only way legally that she can stopped from destroying herself, but the Bradgate Unit in many situations even fails to do that.